The one Anastomosis gastric bypass is also known as the single anastomosis gastric bypass (SAGB), or mini gastric bypass (MGB).
There is a single join (anastomosis) between the new stomach pouch and the small intestine.
For over 25 years, the results from OAGB have shown good, sustained weight loss with improvement in health conditions. As a variant of the Roux en Y gastric bypass, it is a more straight forward operation.
One anastomosis gastric bypass surgery is considered –
- as a primary operation, with a BMI>35
- as a revisional operation, if you’ve had a previous gastric band, gastric sleeve, sleeve gastroplasty, or other weight loss procedure
During your initial consultation, there may be some reasons in your medical history, which may make this operation unsuitable. There are always alternative solutions.
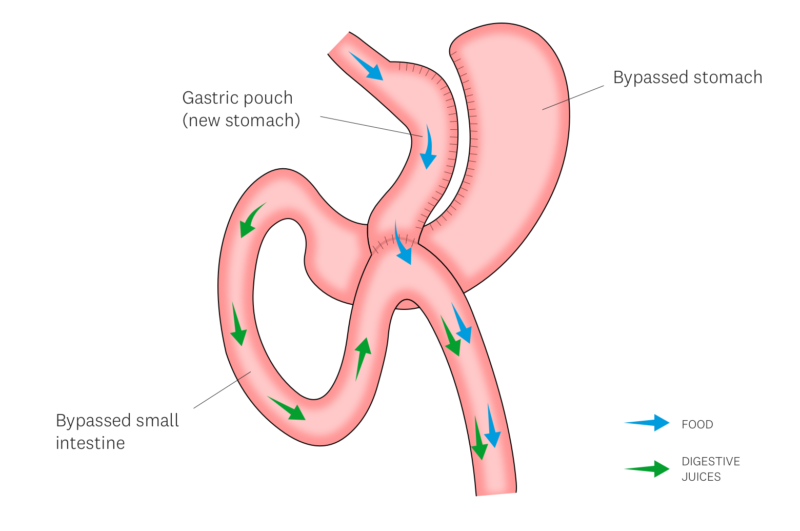
Here’s how the one anastomosis gastric bypass achieves its results:
- Reduced Stomach Size: A section of your stomach is made into a smaller pouch, reducing the amount of food you can eat. This leads to earlier feelings of fullness and ultimately, lower calorie intake.
- Bypassed Intestine: A portion of your small intestine is rerouted, bypassing the original portion of your stomach and a section of the small bowel. This reduces the area available for nutrient absorption, leading to some malabsorption of calories and nutrients.
- Minimally Invasive Procedure: The surgery is typically performed laparoscopically, meaning it uses several small incisions in your upper abdomen. This translates to faster recovery times and less scarring compared to traditional open surgery.
While complications are infrequent, they can occur, and include:
- Anastomotic leak – stomach fluid may leak out into the abdomen at the join created during this procedure, due to failure of the join to heal. This may require further procedures and an extended hospital stay.
- Marginal ulceration – this is an erosion/ulcer of the small bowel joined to the gastric pouch, similar to a stomach ulcer. This may cause pain in the upper abdomen or chest. Most times this is treated with medications. Occasionally, this requires further surgery.
- Stomal stenosis – a narrowing at the join between stomach and small bowel. You may develop vomiting and rapid weight loss, due to inability of food and/or fluids to pass through the narrowed area. Treatment consists of stretching the narrowing up with a balloon, or placement of a stent (tube), and removing it 4 weeks later. Occasionally, this requires further surgery.
- Stomal dilation – a widening at the join between stomach and small bowel. You may feel loss of restriction and be able to eat more. Occasionally, this may require further surgery.
- Internal Hernia – bowel may get trapped in a space created during the formation of the gastric bypass. This may cause a blockage of the small bowel (obstruction) or lead to a lack of blood supply to the small bowel (strangulation). This is an emergency. You must go to your local hospital immediately if you have significant abdominal pain lasting more than one hour, with or without vomiting.
- Bile reflux – bile (fluid produced by the liver to help in digestion of fatty foods) may go up the oesophagus and cause symptoms similar to that of acid reflux/heartburn. Medications will help relieve symptoms. Occasionally, this may require further surgery.
- Dumping syndrome – a cluster of symptoms including feeling sick, rapid heart rate, sweating, flushing, light-headedness, abdominal cramps, and diarrhoea. This is due to eating too much or eating foods high in sugar. Dietary modification will usually fix this issue.
- Nutritional deficiencies – even though you will need to take regular multivitamins, you can become low in certain vitamins or minerals. Additional supplementation may be necessary. You will require lifelong follow-up and blood tests to monitor for potential deficiencies.
Want to continue your OAGB journey?